The Role of Physical Therapy in the Management of Parkinson Disease
Physical therapy (PT) is a part of best practice for people with Parkinson disease (PD). To improve PT interventions for people with PD, the American Physical Therapy Association (APTA) convened a group in 2019 to develop and publish a Clinical Practice Guideline (CPG). The CPG was published in 2021 with the purpose to share which PT interventions have the best evidence to optimize outcomes for people with PD. A group sponsored by the Academy of Neurologic Physical Therapy (ANPT), a subsidiary of the APTA, has been working to spread information about the CPG to other physical therapists and directly to people with PD to strengthen patient-centered care and PT outcomes.
The CPG recommends aerobic exercise, balance training, behavior change approach, community-based exercise, external cueing, integrated care, gait training, resistance training, and task specific training based on high levels of evidence. Definitions of these types of training are in the figure below.
It is likely not possible for a person with PD to engage in all these activities unless physical therapy and rehabilitation become a full-time job! Therefore, physical therapists will select a combination of these interventions based on their clients’ goals and desired outcomes, training preferences, and equipment availability. In addition, physical therapists may apply behavior change approach techniques in conjunction with the interventions they choose for a client. Behavior change approaches can be thought of as coaching between a therapist and client to improve collaborative goal setting and client participation in their rehabilitation.
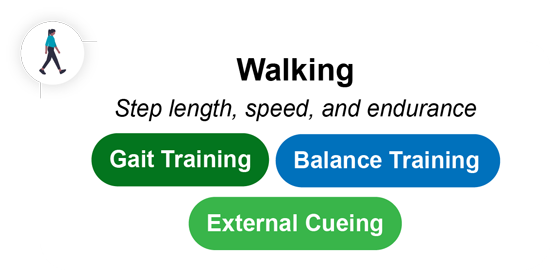
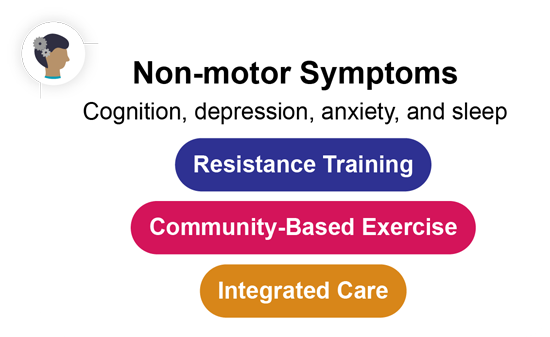
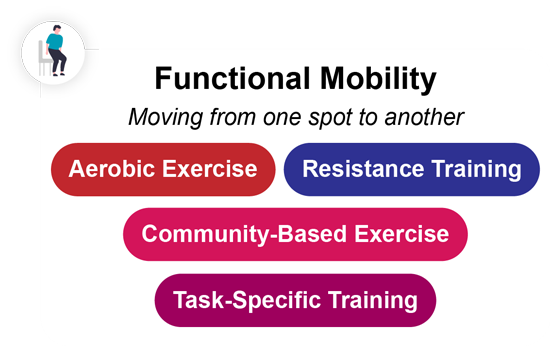
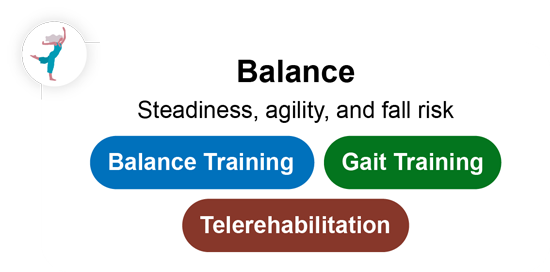
The CPG demonstrates that physical therapy can effectively improve a wide variety of outcomes, including the following: quality of life, functional mobility, motor disease severity, walking, balance, and non-motor symptoms. Quality of life relates to a person’s overall wellbeing and perceived health status. Functional mobility is the ability to move from one spot to another. Motor disease severity encompasses symptoms such as tremor, stiffness, and difficulty moving. Walking involves parameters such as step length, speed, and endurance. Balance includes a person’s steadiness, postural stability, agility, and fall risk. Non-motor symptoms can involve changes in cognition, depression, anxiety, and sleep. People with PD can experience changes in any combination of these categories and can seek out PT to help at any stage of their PD.
A physical therapist should prescribe tailored activities and interventions for each patient. Each activity prescribed by a physical therapist can be thought of as a “pill” tailored to improve a certain limitation or symptom. The colorful “pills” shown below [MR1] illustrate the evidence-based treatment types a therapist may prescribe based on which outcome they are aiming to improve:
The CPG also strongly recommends that exercise interventions are appropriately dosed. For example, flexibility training is recommended as a part of warm-up and cool-down activities but shouldn’t be the entire PT intervention based on the low level of evidence supporting its use to improve main outcomes of interest in PD. Physical therapists should also use behavior change approaches and recommend community-based exercise to help facilitate exercise participation. It is also beneficial if physical therapists work within integrated (interdisciplinary) care teams that include neurology, specialist nurses or social workers, and other rehabilitation disciplines (e.g., occupational and/or speech and language therapy). Physical therapists may use telerehabilitation as a part of their physical therapy practice.
To facilitate dissemination and implementation of this CPG, the ANPT Knowledge Translation Task Force surveyed the knowledge, attitudes, and behaviors of over 300 physical therapists in the United States regarding CPG implementation. In response to the survey results, the task force is creating and disseminating freely available knowledge translation tools for people with PD and physical therapists. These tools focus on appropriate exercise prescription, application of behavior change techniques, and handouts that physical therapists can provide to improve patient/care partner education and outreach. A link to the tools available in the virtual toolbox provided by the ANPT can be accessed here: https://www.neuropt.org/practice-resources/anpt-clinical-practice-guidelines/pt-management-of-parkinson-disease. The clinical practice guideline and educational tools are available in English and Spanish.
The full-length CPG for Physical Therapist Management of Parkinson Disease can be accessed here: https://academic.oup.com/ptj/article/102/4/pzab302/6485202?login=false
1. Osborne, J. A., Botkin, R., Colon-Semenza, C., DeAngelis, T. R., Gallardo, O. G., Kosakowski, H., Martello, J., Pradhan, S., Rafferty, M., Readinger, J. L., Whitt, A. L., & Ellis, T. D. (2022). Physical Therapist Management of Parkinson Disease: A Clinical Practice Guideline From the American Physical Therapy Association. Physical therapy, 102(4), pzab302. https://doi.org/10.1093/ptj/pzab302
by Katherine Marita, DPT, The Ohio State Wexner Medical Center – Columbus, OH USA,
*Miriam Rafferty, DPT, PhDb, Shirley Ryan AbilityLab, Northwestern University – Chicago, IL USA, Deb Kegelmeyer, DPT, MSa, Washington University in St Louis – St. Louis, MO USA, Beth Crowner, DPT, MPPAc and Jay Phillips. *WPC 2023 speaker and poster presenter.
Twitter: @miriamrafferty
Twitter: @APTANeuroPT
Ideas and opinions expressed in this post reflect that of the author solely. They do not reflect the opinions or positions of the World Parkinson Coalition®